Your contraception choices
What is contraception?
Contraception means prevention of pregnancy. Using contraception gives you more control and allows you to decide if, and when, to have children, and allows you to enjoy sex without having to worry about an unplanned pregnancy.
Which contraceptive is right for me?
There are several different methods of contraception available. It is very important to choose a method that best suits your individual needs at the time. Getting accurate information, considering the pros and cons, and talking options over with your partner or partners, are all valuable when you are deciding on the best method for you.
Many factors may affect your choice of a contraceptive method including:
- How effective the method is.
- How easy the method is to use.
- The stage of life you are at.
- Your lifestyle.
- Your relationship status.
- Any possible side effects.
- The cost and availability.
- How easy the method is to reverse.
- Any health issues that may limit some choices.
- Protection against sexually transmissible infections.
Unfortunately, while there is excellent information available online about contraception there is also a lot of inaccurate, confusing, and misleading information out there, as well as plenty of myths. For accurate information it is best to only look at more official sites such as this one.
You can check out the Contraception efficacy guide from Family Planning Association Australia.
Talking with a family planning nurse or doctor about contraceptive methods will give you an opportunity to ask questions and to ensure that you have enough accurate information to choose the method that suits you best. If there is not a family planning clinic in your area, talk to your GP.
Long Acting Reversible Contraceptives (LARCs)
Have you heard about Long Acting Reversible Contraceptives or LARCs? LARCs are methods of contraception that are highly effective, work for a long time, need very little action by you the user, and are quickly reversible when you want to stop using them.
There are four methods of contraception that are classified as LARCs:
- The contraceptive implant.
- The hormone releasing IUD.
- The copper IUD.
- The contraceptive injection.
Contraceptive methods available in Australia
The contraceptive methods that follow are listed from MOST effective to LEAST effective.
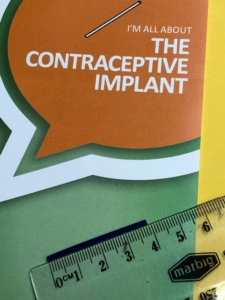
The contraceptive implant
What is the contraceptive implant?
The contraceptive implant (Implanon®) is a small flexible plastic rod (sometimes called ‘the rod’) which is inserted under the skin on the underside of the upper arm. It releases a hormone called progestogen continuously.
How does the contraceptive implant work?
The contraceptive implant works mainly by stopping an egg being released from the ovary (ovulation) which prevents pregnancy occurring. It also increases the thickness of mucus in the cervix which make it hard for any sperm to get through and fertilise an egg.
How long does the contraceptive implant last?
The contraceptive implant is a LARC and works for 3 years.
How effective is the contraceptive implant?
The contraceptive implant is over 99% effective.
Who can use the contraceptive implant?
The contraceptive implant is suitable for most women to use. Your doctor will be able to help you decide if it is suitable for you.
There are some women for who it is not suitable, these include the following:
- Women who might be pregnant.
- Women who have had breast cancer or reproductive organ cancers.
- Women with severe liver disease.
- Women who have undiagnosed abnormal vaginal bleeding.
- Women on certain medications which may interfere with the action of the contraceptive implant. Your doctor will discuss this with you.
What are the advantages of the contraceptive implant?
- It gives you 3 years of effective contraception with no need to do anything on a daily basis.
- It gives you contraceptive cover straight away if it is inserted in the first five days of your cycle.
- It can be removed if side effects are not acceptable or pregnancy is desired.
- Normal fertility returns quickly after removal.
- It is a low-cost method of contraception.
- It can be used by breastfeeding women.
What are the disadvantages of the contraceptive implant?
- It requires a minor surgical procedure to insert and remove.
- It does not provide protection against sexually transmissible infections.
What are the possible side effects of the contraceptive implant?
The most common side effect of the contraceptive implant are changes to menstrual bleeding.
These changes can include:
- Infrequent spotting or bleeding.
- Prolonged or frequent spotting or bleeding.
- No bleeding.
Other possible side effects include:
- Headache.
- Breast discomfort.
- Acne may develop or worsen, although some women may find that acne improves.
- Local reactions at the site of the insertion (see possible risks of insertion).
- Some women report weight changes or mood changes, but available evidence does not support the idea that the implant is a direct cause of these.
How and when is the contraceptive implant inserted and removed?
The implant is inserted by a doctor or nurse who has been specially trained to do this procedure. The insertion is a simple procedure which involves a small injection of local anaesthetic to numb the skin, then the implant is inserted just under the skin in the underside of your upper arm. A crepe bandage will be placed around that part of your arm for 24 hours to reduce swelling and bruising and to reduce any risk of infection.
The implant is usually inserted in the first five days of your period but can be inserted at other times if there is no chance you could be pregnant. When it is inserted within the first 5 days of your period it is effective immediately. When it is inserted at other times in your cycle it will take 7 days to be effective. It is safe to have it inserted following the birth of a baby.
The implant can be left in place for three years, after this time it will need to be replaced. It can be removed earlier if desired. Removal is usually a simple procedure which involves a small amount of local anaesthetic to numb the skin before a very small incision is made and the implant is removed.
Possible risks of insertion are unusual. These include:
- Bruising, soreness, infection.
- Possible scarring at the site of the insertion.
- Possible difficulty removing the implant.
- Allergy to the local anaesthetic or to the implant itself.
Where can I get the contraceptive implant?
The contraceptive implant is available through family planning clinics, including SHFPACT, as well as through most GPs and gynaecologists.
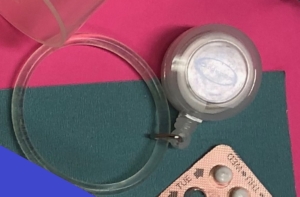
Intrauterine Devices (IUDs)
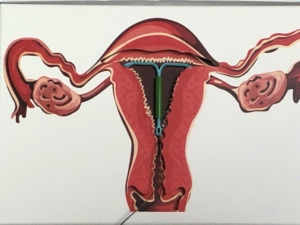
What are IUDs?
IUDs are small devices that are placed in the uterus (womb) to prevent pregnancy. There are two types of IUDs in Australia: the hormone releasing IUD, and the copper IUD.
IUDs need to be inserted by a doctor who has been trained in doing this.
The hormone releasing IUD

What is the hormone releasing IUD?
The hormone releasing IUD (Mirena®) is a small T shaped plastic device that has a hormone called Levonorgestrel in the stem. Levonorgestrel is a type of progestogen and a very small amount of this is released continuously over 5 years.
How does the hormone releasing IUD work?
It works by interfering with sperm movement, thickening the mucous in the cervix so that sperm cannot enter the uterus (womb), and thinning and stabilising the lining of the uterus making it unsuitable for pregnancy.
How long does the hormone releasing IUD last?
The hormone releasing IUD is a LARC and lasts for 5 years.
How effective is the hormone releasing IUD?
The hormone releasing IUD is over 99% effective.
Who can use the hormone releasing IUD?
Most women can use the hormone releasing IUD however there are situations where you may not be able to use an IUD. These include:
- If you have unexplained vaginal bleeding.
- If you have an infection in the uterus or pelvic inflammatory disease (PID).
- If the shape of your uterus means that insertion is not possible (rare).
- If you have breast cancer or have had breast cancer.
What are the advantages of the hormone releasing IUD?
- It is a highly effective contraceptive (99.8%).
- It does not require any day to day action.
- It is long acting.
- The effect is rapidly reversible after removal.
- It is a very cost-effective method over time.
- It can be used by breastfeeding women.
- It decreases menstrual bleeding and pain (many women experience very light periods or no periods).
- It can be used to assist in the management of endometriosis and heavy menstrual bleeding.
What are the disadvantages of the hormone releasing IUD?
- It must be inserted and removed by a doctor.
- As with any procedure there is always a small risk of complications.
- The insertion procedure can be uncomfortable.
- IUDs provide no protection against sexually transmissible infections (STIs).
- You may experience light bleeding and spotting for 3 to 6 months after insertion.
- Your periods may be irregular.
- Some women may have factors in the shape of their uterus that prevent IUD insertion, and this may not be apparent until insertion is attempted.
What are the possible problems which may occur with a hormone releasing IUD?
- There is a very small risk of pregnancy occurring with an IUD (less than 1 in 100). If pregnancy does occur there is a slightly increased risk of it occurring in the fallopian tube.
- Infection: There is a small risk of infection at the time of insertion (about 1 in 500).
- Expulsion: In about 5% of cases the uterus will expel the device. Women need to check that the IUD is still in place by feeling for the IUD string after each period. If the string is not present this may indicate that the IUD has moved or been expelled.
- Perforation: This is a rare event (approximately 2 in 1000 insertions) which occurs when the IUD passes through the wall of the uterus into the pelvic area. This requires surgery under a general anaesthetic to remove the IUD.
How is a hormone releasing IUD removed?
Removal of an IUD is done by a doctor. It is a relatively quick and straightforward procedure.
Where can I get a hormone releasing IUD?
IUDs are only inserted by doctors, nurse practitioners, and nurses who have done IUD training. Family planning clinics provide IUD insertion services. Some GPs and most gynaecologists also provide this service. There are also some clinics that will insert IUDs under sedation.
What happens in the IUD insertion process?
Your first consultation:
- This will depend on where you have your IUD inserted, however first you will need to see a doctor to have an initial consultation and to determine if a hormone releasing IUD is a suitable option for you. You will be given information about the procedure and a prescription for the IUD will then be given to you. You will need to go the chemist and have this filled then you need to bring the IUD with you on the day of insertion. Some clinics stock hormone releasing IUDs and the cost will then be included in the consultation.
- The hormone releasing IUD needs to be inserted on day 1 to 7 of your menstrual cycle (day one being the first day of your period) or at any time if you are currently using the oral contraceptive pill or another reliable method of contraception.
- Following your initial consultation you will need to make an appointment for the insertion.
The insertion:
- The doctor will talk through the procedure and make sure the process is clear.
- An uncomplicated insertion procedure takes about 15 mins. Depending where you have the insertion you may be asked to stay at the clinic for a minimum of 20 minutes following the procedure. If you are not feeling well, you will be asked to remain until the staff caring for you feel that you are well enough to leave.
Following the insertion:
- You will be given information about what to expect afterwards and given a follow up appointment about 4 – 8 weeks later to make sure that everything is ok.
- It is common to experience some bleeding and cramping in the first 24 hours after insertion. This should settle quite quickly, and you should be fine to return to normal activities the following day.
The copper IUD

What is the copper IUD?
The copper IUD is a small plastic T shaped device that has copper wrapped around the stem.
It does not contain any hormones.
How does the copper IUD work?
The copper IUD prevents fertilisation by interfering with sperm movement and also by preventing implantation of a fertilised egg.
How long does the copper IUD last?
The copper IUD is a LARC and lasts for 5 or 10 years depending on the type.
How effective is the copper IUD?
The copper IUD is over 99% effective.
Who can use the copper IUD?
Most women can use the copper IUD, however there are situations where you may not be able to use an IUD.
These include:
- If you have unexplained vaginal bleeding.
- If you have an infection in the uterus or pelvic inflammatory disease (PID).
- If the shape of your uterus means that insertion is not possible (rare).
What are the advantages of the copper IUD?
- It is a highly effective contraceptive (99.8%).
- It does not require any day to day action.
- It is long acting.
- It is effective immediately.
- The effect is rapidly reversible after removal.
- It is a very cost-effective method over time.
- It can be used by breastfeeding women.
- It does not contain any hormones so is suitable for women who cannot, or do not want to use a hormonal contraceptive.
What are the disadvantages of the copper IUD?
- It must be inserted and removed by a doctor.
- As with any procedure there is always a small risk of complications.
- The insertion procedure can be uncomfortable.
- It can make periods heavier and more painful.
- IUDs provide no protection against sexually transmissible infections (STIs).
- Some women may have factors in the shape of their uterus that prevent IUD insertion, and this may not be apparent until insertion is attempted.
What are the possible problems which may occur with a copper IUD?
- There is a very small risk of pregnancy occurring with an IUD (less than 1 in 100). If pregnancy does occur there is a slightly increased risk of it occurring in the fallopian tube.
- Infection: There is a small risk of infection at the time of insertion (about 1 in 500).
- Expulsion: In about 5% of cases the uterus will expel the device. Women need to check that the IUD is still in place by feeling for the IUD string after each period. If the string is not present this may indicate that the IUD has moved or been expelled.
- Perforation: This is a rare event (approximately 2 in 1000 insertions) which occurs when the IUD passes through the wall of the uterus into the pelvic area. This will require surgery under a general anaesthetic to remove the IUD.
How is a copper IUD removed?
Removal of an IUD is done by a doctor. It is a relatively quick and straightforward procedure.
Where can I get a copper IUD?
IUDs are only inserted by doctors, nurse practitioners, and nurses who have done specialised IUD training. Family planning clinics provide IUD insertion services. Some GPs and most gynaecologists also provide this service. There are also some clinics that will insert IUDs under sedation.
What happens in the IUD insertion process?
Your first consultation:
- This will depend on where you have it inserted however first you will need to see a doctor to have an initial consultation and to determine if a hormone releasing IUD is a suitable option for you. You will be given information about the procedure.
- The copper IUD is usually inserted on day 1 to 7 of your menstrual cycle but can be inserted up to day 12 (day 1 being the first day of your period), or at any time if you are currently using the oral contraceptive pill or another reliable method of contraception.
- Following your initial consultation you will need to make an appointment for the insertion.
The insertion:
- The doctor will run through the procedure and make sure the process is clear.
- An uncomplicated insertion procedure takes about 15 mins. Depending where you have the insertion you may be asked to stay at the clinic for a minimum of 20 minutes following the procedure. If you are not feeling well, you will be asked to remain until the staff caring for you feel that you are well enough to leave.
Following the insertion:
- You will be given information about what to expect afterwards and given a follow up appointment about 4 – 8 weeks later to make sure that everything is ok.
- It is common to experience some bleeding and cramping in the first 24 hours after insertion. This should settle quite quickly, and you should be fine to return to normal activities the following day.
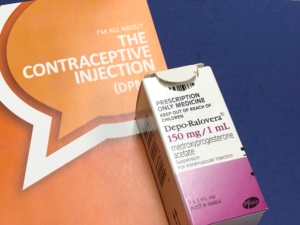
The contraceptive injection
The combined oral contraceptive pill (the pill)
What is the pill?
The combined oral contraceptive pill is commonly referred to as ‘the pill’. It is a pill that contains two hormones: oestrogen and progestogen, and must be taken every day. The pill is usually taken for three weeks then sugar pills are taken for one week before starting a new pill pack. There are many different types of the pill available and your doctor can help find one that suits you.
How does it work?
The pill works by preventing ovulation (release of an egg by the ovary). It also thickens the mucous in the cervix.
How effective is it?
The pill is 93% effective.
How is it taken?
The pill is taken by mouth every day. Most pill types come in a box of 3 to 4 sachets which each contain a month’s supply of pills. The pill sachet contains active pills (pills containing the hormones) and inactive or sugar pills (which help you to keep the habit of taking the pill every day). It is quite acceptable to skip the sugar pills and take the hormone pills continuously for two or three packs in a row. This is quite safe to do. The only side effect may be some spotting if you skip several periods.
Who can use the pill?
Most women can use the pill, however there are situations where the pill cannot be used.
These include:
- If you have had a deep venous thrombosis (blood clot), stroke or heart attack.
- If you have severe liver problems.
- If you get a migraine with aura (is visual or other disturbances starting just before the migraine).
- If you have breast cancer.
The pill may also be unsuitable if:
- You have high blood pressure, diabetes, gall bladder disease, active liver disease, kidney disease, some blood problems.
- If you are on a medication which may interact with the pill.
- If you have had cancer of the breast or cervix.
- If you are over 35 and smoke.
- If you have unexplained bleeding from the vagina.
If any of these conditions apply to you, let your doctor help you decide if the pill is suitable for you.
What are the advantages of the pill?
- It is very effective with correct use.
- It is readily accessible.
- It is easily reversible.
- It gives you a predictable bleeding pattern and allows you to skip periods if you want.
- Periods are usually lighter and shorter on the pill so it can be useful in controlling heavy or painful periods.
- It can be helpful managing premenstrual symptoms.
- It can improve acne, and is sometimes used to treat acne (it can take up to six months for this effect).
What are the disadvantages of the pill?
- It must be taken every day.
- It is less effective if not used perfectly (for example if pills are missed).
- Its effectiveness may be reduced by vomiting or diarrhoea.
- Some types can be expensive.
- It does not provide protection against sexually transmissible infections.
What are the possible side effects of the pill?
- Some of the possible side effects when starting the pill are nausea, breast tenderness, headaches, and acne. These usually settle quite quickly, however if you do have any of these side effects and they don’t settle, talk to your doctor about trying another type of pill.
- While some women report changes in mood there is no evidence that the pill effects mood.
- There is no evidence that the pill causes any weight gain and some types of the pill can actually cause a small weight loss.
- There is no evidence that the pill has a definite effect on sexual function. Some women have reported reduced libido, whereas others report increased interest in sex, particularly in relation to lack of anxiety about unplanned pregnancy.
- Serious health problems caused by the pill are very rare -— the most significant of these is blood clotting. Symptoms of this are severe sudden chest pain, severe pain or swelling in one leg, sudden blurred vision or loss of sight, slurring of speech or sudden severe headache. If you have any of these symptoms contact your doctor immediately.
- Your risk of developing a blood clot is increased when you are not mobile for an extended period of time e.g. sitting in a car or airplane on a long trip, or if you are planning to have surgery which means you may not be mobile for a while. Please talk to your doctor if you are planning any of these.
As well as being a contraceptive, the pill has other health benefits. When on the pill you are less likely to develop a serious pelvic infection, cancer of the ovary, cancer of the endometrium (lining of the womb), cancer of the bowel, anaemia, non-cancerous breast lumps, and cysts of the ovary.
Are there different types of the pill available?
Yes there are many different types of the combined pill on the market. There are some differences between the types of pills available and it may take a few trials to find the one most suitable one for you. Don’t be afraid to discuss your options with your doctor and to keep trying until you find one that suits you best.
Where can I get it?
The pill needs to be prescribed by a doctor. You can see a GP or a family planning doctor who can discuss your suitability for the pill.
What should I do if I miss a pill or pills?
- If you are less than 24 hours late taking your pill (so it’s not more than 48 hours since you took your last pill), take your pill as soon as you remember, and then take the next one at the usual time. This may mean taking 2 pills on the same day. You will still be protected against pregnancy.
- If you are more than 24 hours late taking your pill (so it’s more than 48 hours since you took your last pill) you need to take the most recently missed pill as soon as you remember, and then take the next one at the usual time, this may mean taking 2 pills on the same day. (If you have missed more than 2 pills discard any other pills-don’t take more than 2 pills at once). Then you will need to use condoms or avoid sex for the next 7 days.
- If it is less than 7 days since your last sugar pills you might be at risk of pregnancy and may need to use emergency contraception (see the section on emergency contraception).
- If there is less than 7 days before your next sugar pills, skip them and go straight onto the hormone pills in the next packet.
IF YOU ARE WORRIED ABOUT WHAT YOU SHOULD DO, CALL YOUR LOCAL FAMILY PLANING CLINIC AND TALK TO A NURSE.
The progestogen only pill (mini pill)
What is the mini pill?
The mini pill is a pill that contains only progestogen.
How does it work?
It works by thickening the mucous in the cervix and preventing sperm entering the uterus (womb).
How is it used?
The mini pill must be taken every day and at the SAME TIME each day. It is taken continuously with no break.
How effective is it?
The mini pill is 93% effective.
Who can use the mini pill?
Most women can use the mini pill, however there are situations where the mini pill cannot be used.
These include:
- If you have severe liver problems.
- If you have breast cancer.
What are the advantages of the mini pill?
- It is suitable for most women.
- It is readily accessible.
- It is easily reversible.
- It can be used by women who can’t take oestrogen.
- It can be used when breastfeeding.
What are the disadvantages of the pill?
- It must be taken at the same time every day.
- It is less effective if not used perfectly (for example if pills are missed).
- It can cause irregular and unpredictable bleeding.
- It does not provide protection against sexually transmissible infections.
What are the side effects of the mini pill?
The mini pill has few side effects but the main one Is an irregular cycle. The majority of women taking the mini pill will have changes to their menstrual cycle. This may Include Irregular bleeding or no periods. Some women continue to have a regular cycle.
Where can I get the mini pill?
The mini pill needs to be prescribed by a doctor. You can see a GP or a family planning doctor who can discuss your suitability.
What should I do if I miss a pill or pills?
The progestogen only pill needs to be taken at the same time every day to be effective.
- If you are less than 3 hours late taking your pill, it is a late pill not a missed pill and it will still work.
- If you are more than 3 hours late taking your pill, take it as soon as you remember (this may mean you take 2 pills at the same time). You should use condoms or not have sex for three days from when you start taking it again.
- If you had sex any time after you missed the first pill you should consider using emergency contraception.(See section on Emergency Contraception)
IF YOU ARE WORRIED ABOUT WHAT YOU SHOULD DO, CALL YOUR LOCAL FAMILY PLANING CLINIC AND TALK TO A NURSE.
Condoms

What are condoms?
Condoms are a barrier method of contraception that work by stopping semen entering the vagina during intercourse. They are the only contraception that also provide protection from sexually transmissible infections.
External condoms (male condoms)

The male condom is a sheath made of thin, strong latex, polyurethane, or polyisoprene which is rolled onto the erect penis before vaginal, anal or oral sex. It can only be used once and is then discarded. Latex condoms are the most commonly available condoms.
How effective are they?
Male condoms are 88% effective.
What are the advantages of the male condom?
- They provide protection against sexually transmissible infections (STIs).
- They are easy to get.
- They are relatively affordable.
- You only need to use them as needed.
- They allow the male partner to participate in and have more control over contraception.
- They can be used with other methods of contraception to increase effectiveness and add protection from STIs.
- There are no medical reasons not to use condoms other than allergy to what they are made of (such as latex allergy).
- They have no side effects.
What are the disadvantages the male condom?
- They are less effective than other methods (particularly because they can break or slip off)
- The interruption to sexual activity can be a concern for some people.
- Some people complain of reduced sensitivity during sexual activity.
- Some people may experience difficulties with erections (this can sometimes be helped by practicing using condoms before any partnered sexual activity, especially for younger people).
- Those whose erections are less firm may find it a little difficult to use condoms.
- A small number of people are sensitive to latex or lubricant. Non-latex condoms (polyurethane and polyisoprene) are available for people with latex allergies.
- Latex condoms and polyisoprene condoms must not be used with oil based lubricants.
Using lubricants with condoms.
While most condoms are already lubricated, additional water-based lubricant is always recommended as this will increase comfort and help prevent breakages. Water-based lubricants are available from pharmacies, supermarkets, online, and in sex shops. A number of brands are available so find one that suits. Saliva (spit) is not usually slippery enough to use but may help if nothing else is available.
Oil-based lubricants can weaken latex condoms, and should not be used. These include petroleum jelly (e.g. Vaseline), cooking oil, baby oil, suntan oil, massage oil, hand lotions or creams.
Where can I get male condoms?
Male condoms are available from supermarkets, pharmacies, clinics, sex shops, and vending machines.
Internal condoms (female condoms)

The female condom is a polyurethane sheath which is inserted into the vagina before sexual intercourse. It is about 15cm long and has two flexible rings to keep it in place. It can only be used once and is then discarded.
How effective are they?
Female condoms are 79% effective.
What are the advantages of the female condom?
- They provide protection against sexually transmissible infections (STIs).
- You only need to use them as needed.
- They can be inserted up to 8 hours prior to intercourse so don’t interfere with spontaneity.
- They provide greater sensation.
- They can be used with other methods of contraception to increase effectiveness and add protection from STIs.
- There is very little risk of allergy to them.
- They have no side effects.
What are the disadvantages the female condom?
- They are less effective than other contraceptive methods.
- They can be difficult to get.
- They are more expensive than male condoms.
- Some women find insertion and removal difficult.
- They can make a slight noise during sex.
Where can I get female condoms?
Femidom is the only brand currently available in Australia. They are available to order online and from some sex shops.
Emergency contraceptive pills

There are two oral emergency contraceptives available in Australia:
Levonorgestrel and Ulipristal Acetate. Both of these work by preventing or delaying ovulation (ovulation is the release of an egg by the ovary). The sooner you take them the more effective they are. They are both safe, well tolerated medications, do not affect future fertility, do not cause abortion and cannot effect an established pregnancy. For more information see Emergency contraception.
The contraceptive vaginal ring (NuvaRing®)
What is the contraceptive vaginal ring?
The contraceptive vaginal ring is a plastic ring that is placed in the vagina. It is very similar to the pill and contains two hormones, oestrogen and progestogen.
How does it work?
The contraceptive vaginal ring works in the same way the pill does, by preventing ovulation (release of an egg by the ovary). It also thickens the mucus in the cervix.
How long does it last?
It lasts for three weeks, is removed for a week, then replaced with a new one.
How effective is it?
The contraceptive vaginal ring is 93% effective.
How is it used?
You place the contraceptive vaginal ring into the vagina, leave it for 3 weeks, remove it for one week then replace it with a new ring.
Who can use the contraceptive vaginal ring?
Most women can use the contraceptive vaginal ring, however, similar to the pill there are situations where it cannot be used.
These include:
- If you have had a deep venous thrombosis (blood clot), stroke or heart attack.
- If you have severe liver problems.
- If you get a migraine with aura (is visual or other disturbances starting just before the migraine).
- If you have breast cancer.
The contraceptive vaginal ring may also be unsuitable if:
- You have high blood pressure, diabetes, gall bladder disease, active liver disease, kidney disease, some blood problems.
- If you are on certain medication which may interact with the vaginal ring (your doctor will discuss this with you).
- If you have had cancer of the breast or cervix.
- If you are over 35 and smoke.
- If you have unexplained bleeding from the vagina.
If any of these conditions apply to you, let your doctor help you decide if the pill is suitable for you.
What are the advantages of the contraceptive vaginal ring?
- It is very effective with correct use.
- It is readily accessible.
- It is easily reversible.
- You don’t need to take something daily, it only needs to be removed every 3 weeks then replaced a week later.
- It is not affected by vomiting or diarrhoea.
- It gives you a predictable bleeding pattern and allows you to skip periods if you want.
- It can be useful in reducing heavy or painful periods.
- It can be helpful in managing premenstrual symptoms.
- It can be helpful in managing acne.
What are the disadvantages of the contraceptive vaginal ring?
- You need to insert something into the vagina.
- You need to remember to take it out every 3 weeks then replace it with a new one a week later.
- It is less effective if not used perfectly (for example if you forget to replace it).
- It can be fairly expensive.
- It does not provide protection against sexually transmissible infections.
What are the possible side effects of the contraceptive vaginal ring?
- Some of the possible side effects when starting the vaginal ring are nausea, breast tenderness, headaches, and acne.
- There is no evidence that the vaginal ring affects mood, causes any weight gain, or has an effect on sexual function.
- Serious health problems caused by the contraceptive vaginal ring are very rare -— the most significant of these is blood clotting. Symptoms of this are severe sudden chest pain, severe pain or swelling in one leg, sudden blurred vision or loss of sight, slurring of speech or sudden severe headache. If you have any of these symptoms contact your doctor immediately.
- Your risk of developing a blood clot is increased when you are not mobile for an extended period of time e.g. sitting in a car or airplane on a long trip, or if you are planning to have surgery. Please talk to your doctor if you are planning any of these.
- As well as being a contraceptive, the vaginal rig has other health benefits. When using the vaginal ring you are less likely to develop a serious pelvic infection, cancer of the ovary, cancer of the endometrium (lining of the womb), cancer of the bowel, anaemia, non-cancerous breast lumps, and cysts of the ovary.
Where can I get it?
The vaginal ring needs to be prescribed by a doctor. You can see a GP or a family planning doctor who can discuss your suitability.
The diaphragm
What is the diaphragm?
The diaphragm is a dome of soft silicone with a firm, flexible rim which is placed inside the vagina to cover the cervix (the lower part of the uterus or womb). There are several types of diaphragm available including the Omniflex and the Caya diaphragm.
How does it work?
The diaphragm provides a barrier that prevent sperm getting into the uterus and fertilising an egg. When sperm are trapped in the acidic environment of the vagina they die within 6 hours.
How is it used?
It is inserted into the vagina before intercourse and is then left in place for a minimum of six hours afterwards because it takes 6 hours for sperm to die in the acid environment of the vagina as mentioned above.
How effective is the diaphragm?
The diaphragm is 82% effective.
The 3 most important factors in effectiveness when using a diaphragm are:
- Using the diaphragm every time you have intercourse.
- Making sure it is covering your cervix every time.
- Leaving it in place for a minimum of 6 hours after intercourse.
What are the advantages of the diaphragm?
- They are suitable for those who cannot, or choose not to use a hormonal contraceptive or an IUD.
- They are suitable when breastfeeding.
- They can be used as needed at the time of sex.
- They last for up to 2 years before they need replacing.
- They can be used in conjunction with fertility awareness methods.
What are the disadvantages of the diaphragm?
- They have a higher failure rate than most other methods of contraception.
- Some may have difficulty using them or may not like putting them into the vagina.
- They may not be suitable for some people for anatomical or medical reasons.
- They do not provide protection against sexually transmissible infections.
Where can I get a diaphragm?
Diaphragms should be fitted by a specially trained nurse or doctor (usually at a family planning clinic) to make sure that a diaphragm is suitable for you and to find what size is correct for you.
They can then be ordered online. Some types are not available in Australia and need to be ordered from overseas.
Sterilisation
What is sterilisation?
Sterilisation is a permanent method of contraception. Most doctors who perform sterilisation will discuss the reasons you want this permanent form of contraception. Sterilisation is rarely performed on people under the age of 30.
Male sterilisation (vasectomy)
Vasectomy involves a minor surgical procedure performed by a specially trained doctor that involves cutting the vas deferens (the small tubes leading from the testes).
When is it effective?
Vasectomy is effective 3 months after the procedure.
How does vasectomy work?
It works by preventing sperm entering the ejaculate (cum).
How effective is it?
Vasectomy is over 99% effective.
What are the advantages of vasectomy?
- It is a highly effective contraceptive method.
- It is a very simple and safe surgical procedure.
- It can be done in a GPs office.
- It allows the male to take responsibility for contraception.
What are the disadvantages of vasectomy?
- Vasectomy requires a surgical procedure with some risks of minor complications.
- It should be considered permanent, may not be reversible.
Where can someone get a vasectomy?
Vasectomies are performed by specially trained GPs, clinics, or specialists. Ask your local family planning clinic or GP for information about where it is available in your area.
Female sterilisation (tubal ligation)
Tubal ligation is a surgical procedure that is done under general anaesthetic and is performed in hospital by a surgeon. It involves blocking the fallopian tubes that transport eggs to the uterus.
When is it effective?
Tubal ligation is effective immediately.
How does a tubal ligation work?
It works by preventing fertilisation by stopping the sperm reaching the egg.
How effective is it?
Tubal ligation is over 99% effective.
What are the advantages of tubal ligation?
- It is a highly effective contraceptive method.
- It has no effect on menstrual cycle.
- It is a permanent method of contraception.
What are the disadvantages of tubal ligation?
- It is a surgical procedure that requires hospitalisation.
- There are risks of surgery such as bleeding and infection.
- There are risks with general anaesthesia.
- It is not reversible.
- There may be a long wait to have the surgery in a public hospital.
- It may be expensive if performed in a private hospital.
Where can I get a tubal ligation?
As mentioned above tubal ligation is a surgical procedure which is performed by a surgeon in a hospital. To see a surgeon to discuss tubal ligation you will first need to see a GP to request a referral to a surgeon who does this procedure.
Fertility awareness methods, lactational amenorrhoea, and withdrawal
Fertility awareness methods (FAM)
What are Fertility Awareness Methods?
Fertility Awareness Based Methods of contraception (sometimes called Natural Family Planning methods) are based on identifying the fertile days of the menstrual cycle in order to avoid a pregnancy.
How do they work?
These methods use an awareness of the fertile phase in the menstrual cycle to indicate when sexual intercourse should be avoided in order to prevent pregnancy. This can include monitoring body temperature, the days of the menstrual cycle, and checking cervical mucus.
How effective are these methods?
FAMs are between 75% and 93% effective.
What are the advantages of fertility awareness methods?
- They are suitable for those whose beliefs mean they cannot or choose not to use another form of contraception.
- They have no side effects.
- There are no contraindications.
- They are useful for learning about your cycle in order to become pregnant.
What are the disadvantages of fertility awareness methods?
- They can be difficult to use and require daily monitoring and recording of physical changes.
- They require a high level of commitment.
- They may require long periods of abstinence.
- It takes 3 to 6 months of using the methods and monitoring cycles to become accurate enough to use.
- They can have a higher failure rate than other methods.
- They do not provide protection against sexually transmissible infections.
Where do I find out more?
It is important to learn how to use these methods correctly before using them to prevent pregnancy.
For more information if you are interested in using these methods see the Australian Council of Natural Family Planning.
Lactational amenorrhoea (LAM)
Lactational amenorrhoea is the use of breastfeeding as a contraceptive method.
How does it work?
Fully breastfeeding an infant under six months produces hormones that stop you ovulating.
For lactational amenorrhoea to be effective women need to meet the following criteria:
- Have given birth less than six months ago.
- Menstrual periods should not have returned after the birth.
- Must be fully breastfeeding and not giving the baby any formula or food.
How effective is LAM?
Used correctly LAM is 98% effective.
Withdrawal
This is the withdrawal of the penis from the vagina before ejaculation.
There are much more effective forms of contraception and withdrawal is generally not recommended.
How effective is withdrawal?
Withdrawal is 78% effective.
For more information
Sexual Health and Family Planning ACT: Contraception options
Family Planning NSW: Contraception
Fact sheets about each contraceptive type available here.
Pages that may interest you
Where to get contraception
Emergency contraception
Cost of contraceptive methods
References
Contraception: An Australian clinical practice handbook 4th Edition.
Guillebaud, J & MacGregor, A. 2013. Contraception: Your questions answered. 6th Edition. Churchill Livingstone